The On-X Valve
Posted:
Updated:
Journey of the Heart 🫀 Series
When getting a prosthetic valve replacement, one thing to consider is the increased risk of forming a blood clot. The risk is significantly decreased when getting a bioprosthetic valve1, but those valves have their own downsides when considering their lifespan. For me, a mechanical valve is the way to go. I have many years of active life yet to live (I hope), and to get a new valve every 10-15 years is not something I want to go through. With a mechanical valve, it can be one-and-done – as long as nothing goes wrong.
Blood clots can form in areas of low blood flow (stasis) in and around mechanical valves, although this has been improved with more modern designs. More modern designs also incorporate newer materials which can be more clot-resistant. No matter what mechanical valve you get, you have to manage your haemostatic factors.
Haemostasis: The mechanism that leads to the cessation of bleeding from a blood vessel. This includes platelet clots, the coagulation cascade, and the final clot.2
For most patients, this looks like taking warfarin daily and measuring your INR semi-regularly.
Blood Clots
When you injure yourself, you typically want a clot to form nice and quickly, of course! The less bleeding, the better. Unfortunately, this rapid clotting can lead to a higher risk of clots around the prosthesis.
In the worst case, these clots can lead to a blockage of the blood vessel (embolism). This can be quite severe in cases where an organ (or section of) is fed through one main vessel. If not remedied, this can lead to death (infarction) of the organ/tissue. With the aortic valve, a clot could travel essentially anywhere before lodging in a blood vessel – this includes the brain.2 A clot in a vessel that feeds the brain is called a stroke and these are about as bad as you are currently imagining.
Among other things, a valve can be blocked or obstructed by a thrombosis (non-travelling clot), vegetation (irregular cell growth) from endocarditis, or a pannus (abnormal layer of fibrovascular tissue) around the wall.


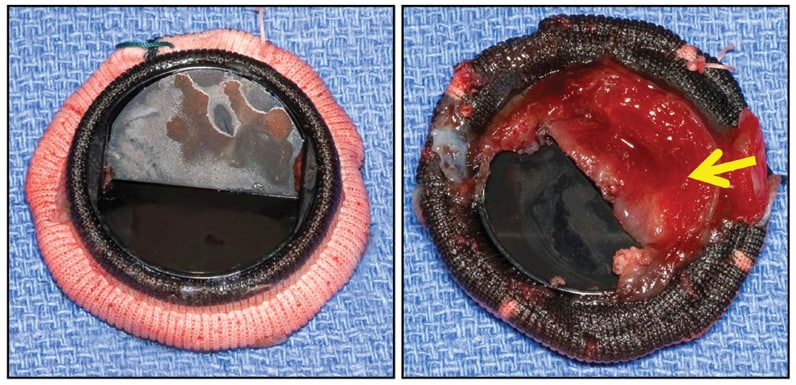
A diagram showing where a pannus and thrombus may form, and their relative morphology, plus real-life images. Sources 1, 2, 3.
Warfarin
It’s important to get a wide variety of vitamins and minerals in your diet, and of particular importance to this discussion, is Vitamin K. Vitamin K is activated by an enzyme and then used in the formation of clotting factors – the things that help stop bleeding. Warfarin inhibits the enzyme which activates Vitamin K, thereby reducing the number of clotting factors in your blood.3 This helps reduce the incidence rate of clot formation on and around a mechanical valve.
You may have already concluded that this may also make you rather bleedy if you get a cut or sustain internal trauma, and you would be right. People on high doses of warfarin often need to take special care in daily life so that they do not put themselves at increased risk of a bleed. This could also prove a problem for people who like to be outdoors, do extreme sports or be very far away from civilisation and medical help.
International Normalised Ratio
This is measured through a relatively simple finger-prick blood test and can be used to assess the risk of bleeding or coagulation status of a patient.
For example, a normal INR range is from around 0.8–1.2. This means that a patient not on anticoagulation medicines would have a prothrombin time of 9.6–14.4 seconds, given an average of 12 seconds. When you take anticoagulation drugs (e.g. warfarin), your time to form a clot increases – sometimes by a lot! The therapeutic range for most valves is between 2.5–3.5, meaning a prothrombin time of 30–42 seconds.4 The higher the INR, the more bleedy you are and the less likely to form a clot on the prosthesis.

Roche CoaguChek INRange System used for patient self-monitoring of INR.
On-X and St Jude
Not all valves are equal. For example, a more modern valve like the On-X has a therapeutic range INR range of 1.5–25. This means that patients with an On-X valve would have to take less warfarin and would be less at risk of adverse bleeding incidents. That is in comparison to, say, the St Jude valve which have a therapeutic range of 2.5-3.56. For me this is great because I like to do sports like rock climbing, trail running, tramping (hiking), moderate mountain climbing and some whitewater kayaking. Being able to take a low warfarin dose and top-up with aspirin (e.g. 80mg)5 would be a huge win.
📷: BMES
That said, because I am getting my valve replaced through the public system here in New Zealand, I have less choice in the valve I will get. In talking to my surgeon, she said that we can aim to use a certain valve, but sometimes when she looks at the heart in the flesh, she doesn’t always feel like she can go ahead with the preferred plan. I am totally cool with that. Of course, I would like an On-X valve over a St Jude (the normal one used at my hospital) due to its lower therapeutic INR range, but I 1000% trust the judgement of my surgeon on the day.
Roudaut, R., Serri, K., & Lafitte, S. (2007). Thrombosis of prosthetic heart valves: diagnosis and therapeutic considerations. Heart (British Cardiac Society), 93(1), 137–142. https://doi.org/10.1136/hrt.2005.071183 ↩︎
LaPelusa A, Dave HD (2023). Physiology, Hemostasis. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK545263/ ↩︎ ↩︎
Patel S, Singh R, Preuss CV, et al. Warfarin. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK470313/ ↩︎
Shikdar S, Vashisht R, Bhattacharya PT. International Normalized Ratio (INR). Treasure Island (FL): StatPearls Publishing; 2023 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK507707/ ↩︎
Bouhout, I., & El-Hamamsy, I. (2019). The Prospective Randomized On-X Valve Anticoagulation Clinical Trial (PROACT): Lower is better, but is it good enough?. Global cardiology science & practice, 2019(1), 2. https://doi.org/10.21542/gcsp.2019.2 ↩︎ ↩︎
Kazuhiko Kido, Jennifer Ball. (2017) Optimal Intensity of Warfarin Therapy in Patients With Mechanical Aortic Valves. https://journals.sagepub.com/doi/full/10.1177/0897190017734765 ↩︎